Epidemiological summary
A total of 189 cases (118 confirmed cases based on positive swab results) were identified during the COVID-19 outbreak between 4th November 2020 to 8th January 2021 at an industrial site in Northern British Colombia (Figure 1). The complete demographic and clinical characteristics of all the 266 individuals investigated during the study period are further shown in Table 1. Our investigation revealed a high proportion of primary cases (n=126, 47.4%) of COVID-19 infection with a high likelihood of being getting infected at the worksite (Please see Appendix for detailed case definition). On the contrary, almost every third individual in the population did not show any signs of potential infection (n=77, 28.9%), hereafter called as control individuals. The findings further revealed that 28.9 % were secondary cases who were most likely infected before joining the worksite. More than 95% of primary and secondary cases were symptomatic. Males were slightly over-represented among cases compared to controls (81.0% vs 74.0%). We also observed that cases, specifically secondary cases, were on average 5-10 years older compared to controls, suggesting old age as a high-risk factor for the infection. In fact, 15 individuals were above 60 years among cases compared to none among the control population. The investigation of health records of cases and controls revealed that prior hospitalization, often used as a proxy of underlying severe illness, did not influence infection susceptibility. Furthermore, only one primary case was admitted to hospital due to COVID-19 related illness during the outbreak. However, no information on the survival of the individual could be obtained from the hospital.
Main investigation findings
With respect to the place of employment, the number of primary and secondary cases were uniformly distributed across all the sites, except at JFJV and Diversified, both located in Kitimat supporting LNG project in Canada. Both the sites reported an unusually high number of primary cases: 28 and 11, suggesting potential sites of the outbreak (i.e., n>10 primary case at each site). Our detailed investigation by following the infection timeline shows that both the places of employment had independent outbreaks with different dates on peaking of confirmed infections (i.e. positive swabs) in both the areas, as shown in Figure 2.
Table 1. Demograpic and clinical characteristics of the study population.
| Population charactersitics | Non-infected (controls) | Primary COVID-19 cases | Secondary COVID-19 cases | Total |
| (N=77) | (N=126) | (N=63) | (N=266) | |
| Age (in years) (continuous) | ||||
| Mean (SD) | 36.2 (8.60) | 41.6 (12.2) | 43.1 (11.8) | 41.3 (11.9) |
| Median [Min, Max] | 37.5 [20.4, 56.1] | 38.6 [19.2, 74.0] | 45.6 [21.5, 69.4] | 39.5 [19.2, 74.0] |
| Missing | 50 (64.9) | 4 (3.2) | 7 (11.1) | 61 (22.9) |
| Age (in years) (categories) | ||||
| 0.0-20.0 | 0 (0) | 2 (1.6) | 0 (0) | 2 (0.8) |
| 20.1-40.0 | 17 (22.1) | 62 (49.2) | 25 (39.7) | 104 (39.1) |
| 40.1-60.0 | 10 (13.0) | 48 (38.1) | 26 (41.3) | 84 (31.6) |
| 60.1-80 | 0 (0) | 10 (7.9) | 5 (7.9) | 15 (5.6) |
| Missing | 50 (64.9) | 4 (3.2) | 7 (11.1) | 61 (22.9) |
| Females, n (%) | 20 (26.0) | 24 (19.0) | 12 (19.0) | 56 (21.1) |
| Number of confirmed cases (positive swabs, n (%))* | 0 (0.0) | 58 (46.0) | 37 (58.7) | 118 (44.4) |
| Presence of symptoms, n (%) | ||||
| Asymptomatic cases | 0 (0) | 6 (4.8) | 7 (11.1) | 13 (4.9) |
| Symptomatic cases | 0 (0) | 120 (95.2) | 56 (88.9) | 176 (77.8) |
| Hospitilization in the last year, n (%) | 3 (3.9) | 5 (4.0) | 2 (3.2) | 10 (3.8) |
| COVID realted hospitalization, n (%) | 1 (1.3) | 1 (0.8) | 0 (0) | 2 (0.8) |
| Indigenous, n (%) | 5 (6.5) | 18 (14.3) | 9 (14.3) | 32 (12.0) |
| Employer, n (%) | ||||
| Diversified | 2 (2.6) | 11 (8.7) | 3 (4.8) | 16 (6.0) |
| JFJV | 27 (35.1) | 28 (22.2) | 17 (27.0) | 72 (27.1) |
| Others | 48 (61.0) | 87 (69.1) | 24 (68.2) | 178 (66.5) |
| Missing | 1 (1.3) | 0 (0) | 0 (0) | 1 (0.4) |
| Job Title, n (%) | ||||
| Carpenter | 6 (7.8) | 13 (10.3) | 4 (6.3) | 23 (8.6) |
| Labourer | 6 (7.8) | 10 (7.9) | 7 (11.1) | 23 (8.6) |
| Others | 65 (84.4) | 103 (81.7) | 52 (82.5) | 220 (82.7) |
| Location / Work area, n (%) | ||||
| CMT2 | 16 (20.8) | 22 (17.5) | 15 (23.8) | 53 (19.9) |
| Field | 16 (20.8) | 12 (9.5) | 5 (7.9) | 33 (12.4) |
| Others | 43 (55.8) | 92 (73.0) | 43 (68.3) | 178 (66.9) |
| Missing | 2 (2.6) | 0 (0) | 0 (0) | 2 (0.8) |
| Work camp accommodation, n (%) | ||||
| CVL | 33 (42.9) | 101 (80.2) | 45 (71.4) | 179 (67.3) |
| HN | 7 (9.1) | 10 (7.9) | 10 (15.9) | 27 (10.2) |
| Local | 37 (48.1) | 15 (11.9) | 8 (12.7) | 60 (22.6) |
| Home Residence, n (%) | ||||
| Calgary AB | 4 (5.2) | 20 (15.9) | 10 (15.9) | 34 (12.8) |
| Edmonton AB | 1 (1.3) | 11 (8.7) | 6 (9.5) | 18 (6.8) |
| Kitamaat BC | 21 (27.3) | 11 (8.9) | 3 (4.8) | 33 (13.2) |
| Others | 51 (66.2) | 84 (66.7) | 44 (69.8) | 181 (68.0) |
| Missing | 1 (1.3) | 0 (0) | 0 (0) | 1 (0.4) |
| Mode of Transportation to Site, n (%) | ||||
| Personal transport | 18 (23.4) | 13 (10.3) | 4 (6.3) | 35 (13.2) |
| YEG Company Charter | 5 (6.5) | 16 (12.7) | 7 (11.1) | 28 (10.5) |
| YYC Company Charter | 1 (1.3) | 16 (12.7) | 8 (12.7) | 25 (9.4) |
| YYC charter | 0 (0) | 10 (7.9) | 1 (1.6) | 11 (4.1) |
| Others | 42 (54.5) | 68 (54.0) | 42 (66.7) | 152 (57.1) |
| Missing | 11 (14.3) | 3 (2.4) | 1 (1.6) | 15 (5.6) |
*23 positive swab cases coutld not be classified into sympomatic or asymptomatic (primary or seondary cases due to lack of information on date of swab collection or visit to the site)
On the contrary, only JFJV had the number of secondary cases in double digits among all the sites. We also observed a high rate of primary infection among carpenters and labourers, which could
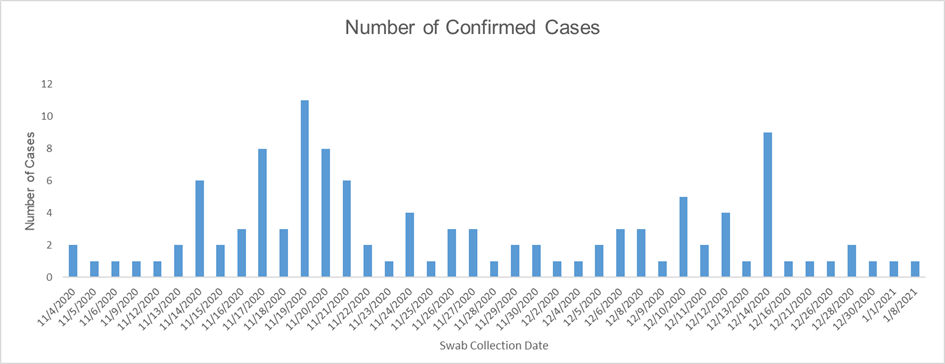
Figure 1. Frequency of confirmed cases during the duration of COVID-19 outbreak.
be attributed to close-contact and teamwork required for such professions. Concerning the work location, individuals working at CMT and those involved in fieldwork were more likely to be infected. An important observation was that most of the cases were residing in civilian localities. On the contrary, among controls, individuals were distributed equally among civilian localities and local work camps.
Most of the workforce comes from other povinces namely Calgary in Alberta povince (12.8%) and Edmonton in Alberta province (6.8%). On the contrary, 12.1% of the population is from Kitimat, in British Colombia. We also observed a trend of a high proportion of primary and secondary cases among individuals coming from Calgary (15.9%), suggesting a possible region that needs to be investigated for the onset of infection. Another important finding was a high prevalence of primary infection among people using charter services for transport. For instance, two large independent clusters of infections were observed among individuals using YEG company charter (n-16, 12.7%) and YYC company charter (n=26; 20.6%). The investigation also showed that many individuals among secondary cases were non-indigenous.
Potential areas of investigation and recommendations
No single underlying symptom could be identified among primary and secondary symptomatic cases. However, the disease clearly infects the upper respiratory tract with symptoms
ranging from fever, cough, sore throat, chills, runny nose, and congestion. Therefore, the role of
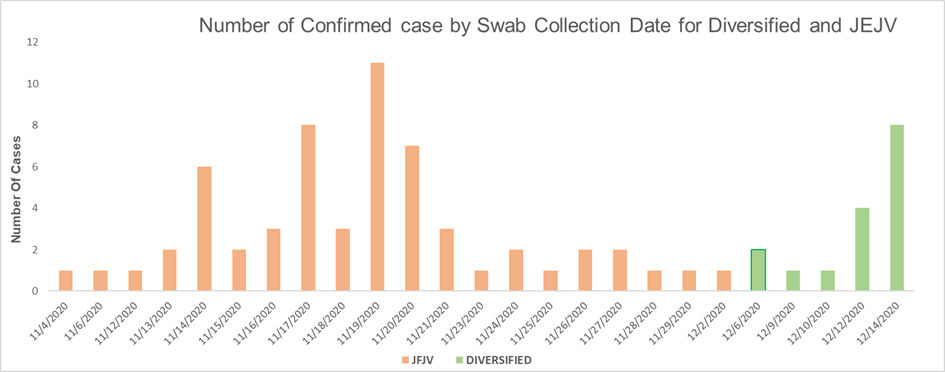
Figure 2. Frequency of confirmed cases from the main outbreak sites (JFJV and Diversified) during the duration of COVID-19 outbreak.
infection spreading through droplets cannot be ruled out and needs further investigation. The results also suggested that non-indigenous may be more susceptible to infection. Calgary in the province of Alberta need to be alerted immediately for a possible breakout among the local community there. The spread of infection among those working or travelling together suggest that the disease is highly contagious. It is therefore recommended to avoid all those activities which increase contact among individuals. This could include working in shifts or remotely wherever possible and using private transport for travelling to the worksite. However, the detection of a small proportion of asymptomatic cases is a dangerous trend as symptomatic individuals are more likely to be tested for the new infection. Therefore, it is likely that the prevalence of the disease reported in the present study may not give the real picture of the extent of spread of this novel virus. The presence of undetected asymptomatic individuals means a need for strict whole population-based measures to curb the infection quickly. There is a need to protect specifically the elderly population from asymptomatic individuals. Although no deaths have been reported so far, the possibility of infection spreading quickly cannot be ruled out, leading to a significant burden on local clinics. This burden is specifically of great concern because of the ongoing winter season when other infections like influenza are widespread among the community.
Appendix: Definitions
- Case definition
Primary case:
Primary cases are defined as confirmed or epi-linked COVID-19 cases who are epidemiologically linked to the site:
worked or stayed at the associated work site/work camp during their incubation period prior to illness onset (for symptomatic cases)/positive swab collection date (for asymptomatic cases),
AND
most likely source of infection was an exposure at the work site/work camp or during associated activities.
Secondary case:
Secondary cases are defined as confirmed or epi-linked COVID-19 cases who:
did NOT work or stay at the associated work site/work camp during their incubation period prior to illness onset (for symptomatic cases) or positive swab collection date (for asymptomatic cases),
AND
did have household contact or other exposure to a linked primary case and is believed to have acquired infection from this contact.
- Incubation Period (time from exposure to an infection until onset of symptoms): 14 days
- Period of Communicability (period of time during which an individual can transmit infection to others):
For symptomatic cases: 2 days prior to onset until 10 days post onset or symptom resolution, whichever is longer
For asymptomatic cases: 2 days prior to specimen collection date until 10 days after specimen collection date. If the case develops symptoms, until 10 days following symptom onset or symptom resolution, whichever is longer.
- Confimed case: A case with postivie COVID-19 swab test.
- Age of the patient: It was computed on the date of collection of swab.
- Duration of outbreak: Date of fist positive swab detection to the data of last positive swab collection.

Leave a Reply